Breathing and Blood Pressure
High blood pressure is an under-appreciated risk for stroke and cardiovascular diseases. Slow and nasal breathing can lower your blood pressure.
Almost 1.3 billion people are diagnosed with high blood pressure. There are many more people (another 1.1 billion!) that are unaware that they have hypertension (high blood pressure). The WHO estimates that less than half of adults who have hypertension is actually diagnosed and treated. Australian data indicates that 1 in 3 people over 18 have high blood pressure and only 11% is controlled using medication. The prevalence increase after the age of 75 to 8 in 10 people.
What is blood pressure exactly? How do you know if it is high? Why should you care if your blood pressure is a little high?
What is blood pressure?
Pressure, like most things in physics, can be hard to understand. Pressure is defined as the force that a a liquid or gas applies to an area In the case of blood pressure, it can be described as how hard the (liquid) blood is pressing on the walls of the arteries. The arteries can expand a little bit to accommodate a higher pressure, but it has limits. I like to use the analogy of water in a hose pipe. When you open the tap a little bit, water is trickling out - this is low pressure. When you open the tap the right amount, the water flows out in an even flow - the correct pressure. If the tap is opened too much, the pressure is too high and the water is bursting out. You may even find it difficult to control the hosepipe.
How do you know if your blood pressure is high?
Blood pressure is measures in millimeters of mercury (mmHg). To measure blood pressure, an armband is placed around the upper arm - called a cuff. The cuff is inflated with air to completely restrict the blood flow below. There will be no pulse below the cuff for this brief period. Then the pressure is lowered and restriction is slowly released allowing the blood to flow back. The doctor will listen for the heart beat to return as the pressure is released - this is the 1st number. The seconds number is when the heart beat is not as pronounced or quiets down. It is a little bit more complicated and what the doctor is actually listening for is called Korotkoff sounds. These days blood pressure is measured automatically with clever devices, and you can get home for your own personal use at any pharmacy.
There are two readings and the doctor will tell you a top and bottom number for example a normal reading will be “120 over 80” or “120/80 mmHg”. The top number is called systolic and is the highest pressure measure - at the time the heart is contracting and pushing blood into the arteries. The lower number is called diastolic and is the lowest pressure - at the time the heart is at rest, between beats.
Why should you care about high blood pressure?
Blood pressure changes during the day, depending on what you are doing. Is it a function of how much blood you need and how fast. It is lowest when you are sleeping and higher when you are exercising. It can also be higher when you are stressed. The high blood pressure during exercise is not something to worry about (within limits of course). However, if blood pressure is high most or all of the time during the day, it is not a good thing. The higher rate of flow of blood in the arteries can damage the thin walls, especially at branches called bifurcations. Much like cars in a tunnel, if everyone is driving at the speed limit there will be lower chance of crashes. When the cars are driving too fast, the risk of crashing into the walls increase - especially when at tunnel exits.
Normal blood pressure ensures that all organs get the right amount of blood to perform their function. Too little blood can lead to ischemic damage where cells do not get enough oxygen to make energy. The most common symptom of low blood pressure is lightheadedness and in the brain this can lead to declining mental status and lethargy.
The kidneys are especially sensitive to blood pressure, where high pressure cause damage to the tiny blood vessels that can be difficult to reverse with renal failure as the end result. Prolonged high blood pressure increase the risk for cardiovascular diseases including stroke, heart attack and aneurysms. The eyes are another area that can be irreversibly damaged, this is called retinopathy.
There is a host of blood pressure medication for hypertension. There are different classes of drugs including ACE inhibitors, angiotensin-2 receptor blockers (ARBs), calcium channel blockers and diuretics.
Risk factors for high blood pressure include:
older age
genetics
being overweight
being unfit
drinking too much alcohol ( >2 daily for men and >1 for women)
smoking
unmanaged stress.
Of the 7 risk factors listed above, 5 are modifiable through lifestyle. Some are easier to do than others. Lose weight. Be active. Stop smoking. Drink less alcohol. And find ways to increase resilience to daily stress - exercise and sleep are the most important things in this case.
Slow Breathing and Blood Pressure
Medications for hypertension are not always effective and many have side-effects that patients struggle with. Interest are increasing to look for nonpharmacological interventions to treat blood pressure. These can be especially effective in prehypertensive patients. As early as 1959, scientists have investigate the effect of breathing on blood pressure. A Pubmed search of “hypertension” and “slow breathing” lists 396 results.
Gholamrezaei et al. (2019) list two proposed mechanisms for the therapeutic effect namely (1) stimulation of the arterial baroreceptors and (2) increased vagal modulation. In many research experiments volunteers are asked to breathe at a rate of 6 breaths per minute (a frequency of 0.1 Hz). This breathing rate is called Respiratory Sinus Arrhythmia (RSA) and is easily achieved with either 5 second inhale and exhale (5-5) or 4 second inhale followed by 6 second exhale (4-6). The latter is my preference when I guide clients in slow breathing.
Cernes et al. (2017) used a device assisted technique to assists patient to achieve the slower breathing rate. These can include following a dot on a screen or listening to a metronome. In some experiments the patients receive direct biofeedback.
One of the most known papers is a Systematic Review and Meta-analysis (2019) by Ashish Chaddha as first author and David Feldstein as last author. They looked at data of all studies that used interventions methods consisting of <10 breaths/ minute, for >5 minutes per day, on >3 days per week, for >4 weeks duration compared to a control group. Slow breathing reduced systolic blood pressure by ~6 mmHg and diastolic pressure by ~3 mmHg. This is considered a modest reduction and comparable to many medication outcomes.
Slow breathing protocol: <10 bpm | >5 min pd | >3 days pw | >4 wks
Many of you will have listened to the podcast on Huberman Lab with Jack Feldman - a leading scientist in the breathing space. It is well worth a listen.
Slow breathing and HRV
In 2010 Oneda et al. found that slow breathing decrease the sympathetic nerve activity. This finding has been replicated in many studies.
Slow breathing increase the PNS tone (vagal tone), allowing for better recovery from stress.
Our autonomic nervous system (ANS) is divided into two arms: sympathetic and parasympathetic nervous system respectively or SNS and PNS for short. The PNS controls the homeostatic balance and the body at rest: the “rest and digest” function. The main nerve associated with the PNS arm is the vagus nerve. Hence the obsession with vagal tone and vagal stimulation in social media.
The SNS controls the body’s responses to a perceived threat and is responsible for the “fight or flight” response. It is not correct to think that it would be good to “switch off the SNS”. Both signals are always “on”. They each have a time and place to be the dominant signalling tone. When you are exercising you want the SNS to be the dominant tone and when you are sleeping the PNS.
Heart rate variability (HRV) also improved with slower breathing. In short, HRV is the difference in time between heart beats, as shown in the figure below. It is a measure of recovery and a measure of your ANS signalling, a high HRV indicates good recovery (more PNS) and a low HRV indicates high levels of stress (more SNS). I will delve more into the world of HRV in a future post.
Figure 1, show an example of heart rate as measured by an electrocardiogram (ECG). The highest peak is called “R” and the time difference between them is called the RR interval variation. Measuring HRV is actually much more complex with mathematical formulas for different parameters including RMSSD, low frequency, high frequency, and more. Fortunately theses are not critical to understand for our everyday purposes. When there is a lot of variation between the heartbeats, the term “High HRV” is used. A “Low HRV” then means there is a high degree of similarity of time between the beats: a pattern of 1.00, 0.99, 1.01, 0.98, 0.98, 0.99 for example. This explanation is the simplest and most relevant for everyday use.
Nasal Breathing and Blood Pressure
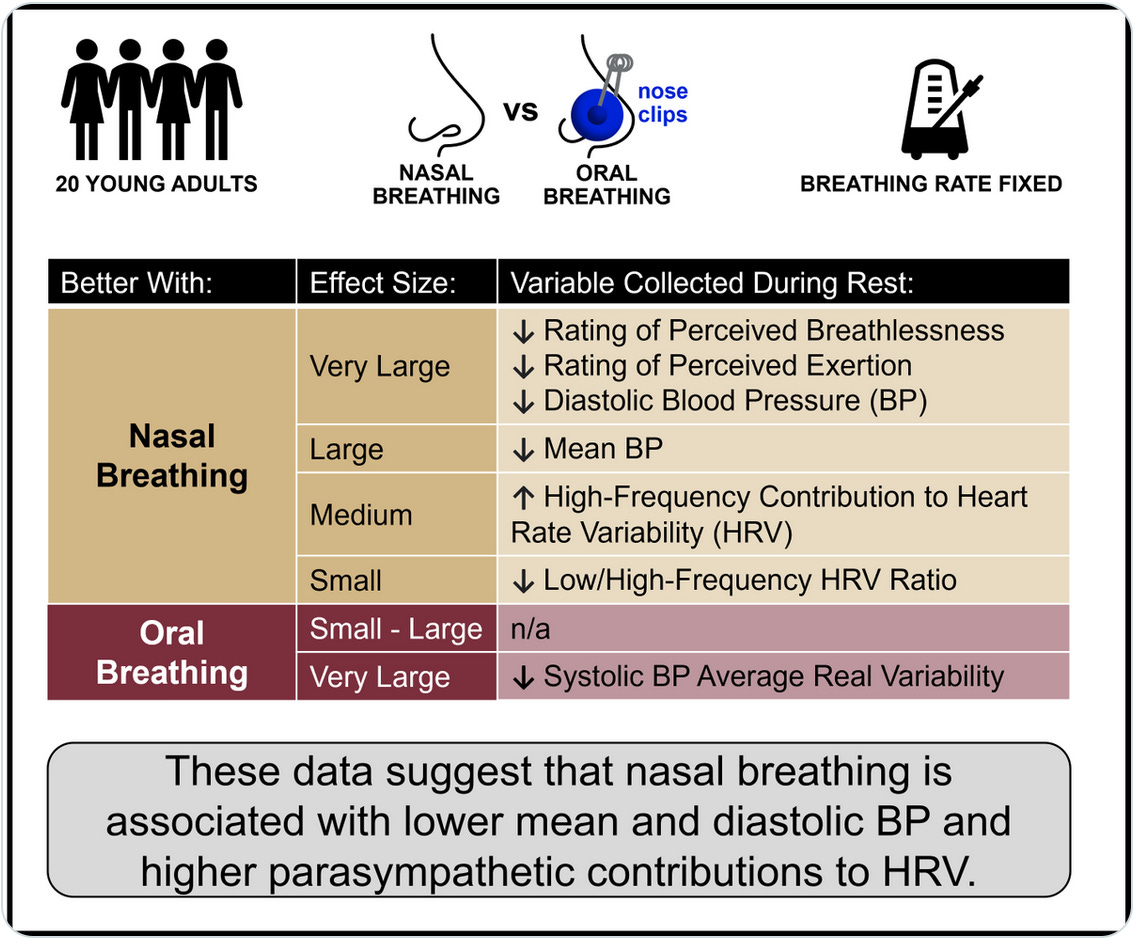
This week (October 2023), a research paper was published by Watso et al. where the effect of nasal breathing on many respiratory and cardiovascular markers was investigated. It was a small study with young healthy adults. The effect of nasal and then oral breathing was assessed at rest, during sub-maximal exercise and during peak-exercise.
The biggest take-away was that nasal breathing at rest for only 5 minutes will have a large effect on lowering blood pressure in healthy young adults. It is not unreasonable to expect that the effect would be similar if not more with hypertensive patients. HRV was increased (improved) with nasal breathing compared to oral breathing.
One of the mechanisms involved is the higher generation of nitric oxide in the airway epithelium during nasal breathing when compared to oral breathing. Nitric oxide is a short lived gas and in the epithelium acts as a signalling molecule to initiate smooth muscle relaxation. In other words the muscles around the blood blood vessels in the airway relax and this allows for a dilation of the blood vessels. When blood vessels dilate, the bigger diameter reduce the pressure. Using the analogy above it is the equivalent of using a bigger hose pipe for the same amount of water resulting in a smoothers flow.
Nasal breathing increase the diaphragm role in breathing, (it is always used), allowing the accessory inhale muscles of the neck and shoulders to rest. With less muscle needed to breathe, there is a lower metabolic (energy) demand.
The data during exercise was less convincing and affected by experimental difficulty of measuring blood pressure, heart rate and other markers while participants are moving. The exercise protocol was conducted on an ergo bicycle.
RPB: rate of perceived breathlessness - “a feeling of not getting enough air”
One of the most interesting results is the effect of nasal breathing during exercise on the subjective marker, rate of perceived breathlessness (RPB). Objective markers are measurable by others or machines for example, heart rate, oxygen saturation and so on. Subjective markers can only be reported by the person experiencing the effect - it is a cognitive assessment and evaluation of emotions or feelings. In other words, “how it feels”. Breathlessness is a key measure to indicate if a person is “getting enough air”. People with asthma will report high breathlessness during an asthma attack. When you exercise to high intensity, you may feel you are not getting enough air and may be gasping for breath - this is also breathlessness. So the harder you work during exercise, the more breathless you may feel.
In this experiment, the participants reported lower RPB with nasal breathing during exercise.
They felt more breathless with mouth breathing than they did with nasal breathing during exercise. I will explore this in future.


Conclusion
High blood pressure is very common and often undiagnosed. It carries a huge risk for chronic disease with potentially crippling outcomes. Lifestyle modifications can in many cases reduce the need for medication: lose weight, exercise and drink less alcohol.
Retraining your breathing is a very simple way to help reduce your blood pressure and improve your stress resilience.
Start with being aware of your breath.
Prioritise nasal breathing.
Until next time
Estelle
Reference:
WHO Hypertension Fact Sheets: https://www.who.int/news-room/fact-sheets/detail/hypertension
Australian Institute for Health and Welfare: Risk Factors for health: Hypertension: https://www.aihw.gov.au/reports/risk-factors/risk-factors-to-health/contents/high-blood-pressure
Australian Bureau of Statistics: Hypertension: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4364.0.55.002~2014-15~Main%20Features~Hypertension~10007
Brzezinski., W. A. (1990). Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. (H. W. Walker HK, Hurst JW,, Ed. 3rd ed.). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK268/
Cernes, R., & Zimlichman, R. (2017). Role of Paced Breathing for Treatment of Hypertension. Curr Hypertens Rep, 19(6), 45. https://doi.org/10.1007/s11906-017-0742-1
Chaddha, A., Modaff, D., Hooper-Lane, C., & Feldstein, D. A. (2019). Device and non-device-guided slow breathing to reduce blood pressure: A systematic review and meta-analysis. Complement Ther Med, 45, 179-184. https://doi.org/10.1016/j.ctim.2019.03.005
Gholamrezaei, A., Van Diest, I., Aziz, Q., Vlaeyen, J. W. S., & Van Oudenhove, L. (2019). Influence of inspiratory threshold load on cardiovascular responses to controlled breathing at 0.1 Hz. Psychophysiology, 56(11), e13447. https://doi.org/10.1111/psyp.13447
Oneda, B., Ortega, K. C., Gusmão, J. L., Araújo, T. G., & Mion, D., Jr. (2010). Sympathetic nerve activity is decreased during device-guided slow breathing. Hypertens Res, 33(7), 708-712. https://doi.org/10.1038/hr.2010.74
Watso, J. C., Cuba, J. N., Boutwell, S. L., Moss, J., Bowerfind, A. K., Fernandez, I. M., Cassette, J. M., May, A. M., & Kirk, K. F. (2023). Acute Nasal Breathing Lowers Diastolic Blood Pressure and Increases Parasympathetic Contributions to Heart Rate Variability in Young Adults. Am J Physiol Regul Integr Comp Physiol. https://doi.org/10.1152/ajpregu.00148.2023