Using Strength Training to reverse Osteopenia. A success story.
Over 16 months a 56y old female improved bone mineral density by over 10% through resistance training.
For easy reading the following post does not contain many technical and medical details. If you are interested in more clinical detail, the data is presented as case report in another post here (will post link soon).
As a Clinical Nutritionist I see many different types of health related challenges. Most often it is sleep. Not this time. About 18 months ago a client came to see me, let’s call her Laura, and her first words to me were “I think I am (stuffed)”. Her words were stronger but I think you get the drift. On my recommendation to be proactive about her long-term health she had a Bone Mineral Density scan (BMD). Laura’s results were borderline for osteoporosis. At the age of 56, her results showed a T-score* of -2.3 for the lower spine and -2.4 and -2.5 for the left and right hips respectively. In other words, the strength of her bones were considered below optimal. This increases her risk of fracture in the event of trauma, typically a fall. Her alarm was not unfounded. A low bone mineral density (BMD) is associated with frailty and with it comes early mortality.
“ Here is my bone mineral density scan - I think I am (stuffed) “
She wanted to know how she could improve her diet to improve the osteoporosis. Most people associate bone health with calcium. And yes, calcium is important as one of the main components of bone. But so are a lot of other nutrients including sufficient protein intake, vitamin D, vitamin K, magnesium, phosphorus, boron, collagen and others. The most well known dietary source of calcium is dairy products like milk, yoghurt and cheese. Other less appreciated foods high in calcium are sardines (with bones) and fortified cereals and orange juice. In this case, Laura’s diet was not the main cause her low BMD. She is a lifelong lover of dairy and her calcium intake was adequate.
Dietary calcium is absorbed in the small intestine and then stored in bones. Unabsorbed calcium is excreted via urine or faeces. The level of calcium in the human body is tightly regulated by hormone signalling. When serum (blood) calcium levels are low, a hormone called parathyroid hormone is secreted by the thyroid gland signalling bones to release calcium, increase the re-absorption in the kidneys and indirectly increase the absorption from the intestines (through another hormone calcitonin). This ensures that the calcium level in the blood is always in the optimum range. In other words you will absorb more calcium from food and excrete less if your calcium levels are low and vice versa. Besides bone strength, calcium has other important roles including regulation of hormonal secretion, nerve signalling and muscle contraction.
Supplements with a high calcium content is not without risk. Mixed evidence show a relationship of high-dose calcium supplements and heart disease, colon polyps and kidney stones. Calcium from supplements is not absorbed as well as from food and can lead to constipation. Vitamin D and vitamin K play crucial roles in the absorption and deposition of calcium.
The typical medication prescribed by medical doctors to increase BMD is Denosumab (Prolia) and comes a long list of side-effects including bone pain, headaches, and a variety of skin related issues. And yes, they do increase the calcium content and make the bones harder. It also makes bones more brittle, much like chalk is hard but brittle. The NIH states that it may increase the risk of breaking thigh bones even if there was no trauma and it may lead to slower healing in the event of a break.**
Compared to chalk, bones are more bendy, it has a certain amount of give on impact, a little spring.
Bones
Cells in our body is constantly being remodelled, this means that old cells are replaced by new ones. Skin cells, the cells lining your gut, muscles cells and bone cells are some examples. The remodelling process is to our advantage because it enables bone to respond and adapt to changing functional demands. In bones the process of breaking down cells is called bone resorption performed by cells called osteoclasts. Cells called osteoblasts are responsible for making new bone tissue.
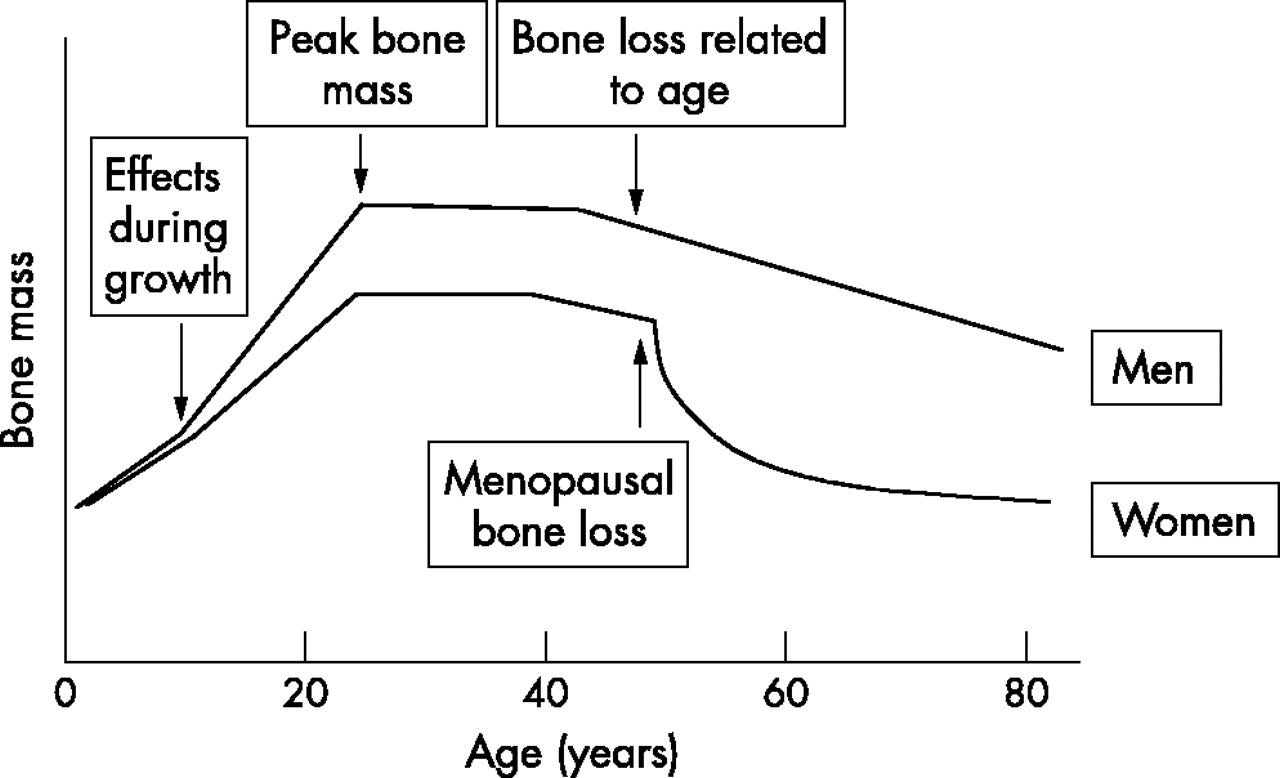
Think about building a wall with bricks, on the one side there is a dedicated bricklayer but on the other side is a guy (with an evil smile?) breaking down the wall. If the building and breaking is at the same rate, the wall will remain stable - the bone density stays the same. As we get older, the bricklayer becomes a bit slower and the wall is slowly getting smaller. For women the rate of bone loss rapidly increases after menopause when oestrogen levels drop. Imagine walking down a gentle hill which then suddenly change into a very steep hill.
The figure below is extracted from Dogan E, Posaci C. Monitoring hormone replacement therapy by biochemical markers of bone metabolism in menopausal women. Postgraduate Medical Journal 2002;78:727-731. BMD with age
Strength training is the best intervention for improving bone density
The best intervention to improve her bone strength is a strength training. Laura needed to start a strength and conditioning program. My words to Laure were: “You need to start lifting weights. It needs to be heavy. Twice a week. For the rest of your life.”
“You need to start lifting weights. It needs to be heavy.
Twice per week. And you cannot stop ever”
Laura was motivated to change but the only exercise she had experience in was jogging when she younger. The thought of picking up weights, much less barbells and plates in a ‘bro-gym’ setting was not appealing. I referred her to a female physiotherapist that was running personal strength training. Laura started with the trainer twice per week. She worked hard, learning new movement patterns, becoming familiar with kettle bells, bar bells, weight plates and dumb bells. These sessions were not the typical F45-style workouts of low weights and high reps. Over time Laura grew to love these sessions.
Over the 18 months her training was interrupted twice. After about three months of training, Laura fainted, hit her head so hard that she required stitches in two places. Not surprisingly, she had a mild concussion. The fainting was as a result of under-hydration during and after a training session. Her training was put on hold for 6 weeks. She returned to training armed with better knowledge about fuelling and hydrating for training.
Approximately six months later, Laura had a second injury. A mirror broke and she received a cut to the top of her right forearm severing several tendons, a nerve and almost through the radial artery. Using her hand was out of the question for many weeks and weight lifting was put on hold. To get some load bearing exercise, Laura started walking with a weight vest. She settled on 15% of her body weight and walked 2-3 times per week. She returned to lifting and formal strength training after 3 months.
16 months later
And then in she had a repeat bone density scan in March 2023 - 16 months after the 1st scan. The results were outstanding. In the words of the radiographer:“ … significant improvement in bone density in the spine of over 10% and in the left femur of 5.5%. In the right femur there has been a strong upward trend of 4.5%. This is an impressive result given that the patient has not been on anti-resorptive therapy…”
“..improvement of 10%…an impressive result..”
Needless to say, Laura was over the moon.
Her determinations and dedication paid off. She did all the work.
To be honest, I was very relieved. I was not sure how much of an improvement in her bone density to expect. During our initial conversation, I proposed that the strength training together with oestrogen replacement can at best slow the rate of decline. Laura opted to trial the lifestyle intervention for 12 months with the understanding that she could start the prescribed bone strengthening medication if the density continues to decline at an unacceptable rate.
Turning the decline into an increase through strength training is almost unheard of. This is partly due to the fact that medication is prescribed as the gold standard of treatment. Research studies will likely not be funded if the control arm does not include the standard treatment as it would be considered unethical to withhold best treatment on randomisation. Teasing out the effect of strength training only is therefore very difficult.
This case is an excellent example of the huge impact that strength training can have on bone density. …..
*T-score compares the BMD to the norm for a healthy young adult age 30 years, where a score of -1 to +1 is considered normal. A T-score of -1 to -2.5 indicates low bone mass (osteopenia) and below -2.5 indicates osteoporosis. NIH Bone Density Scan
Reference:
Anderson, J. J. B., Kruszka, B., Delaney, J. A. C., He, K., Burke, G. L., Alonso, A., Bild, D. E., Budoff, M., & Michos, E. D. (2016). Calcium Intake From Diet and Supplements and the Risk of Coronary Artery Calcification and its Progression Among Older Adults: 10‐Year Follow‐up of the Multi‐Ethnic Study of Atherosclerosis (MESA). Journal of the American Heart Association, 5(10), e003815. https://doi.org/doi:10.1161/JAHA.116.003815
Dogan, E., & Posaci, C. (2002). Monitoring hormone replacement therapy by biochemical markers of bone metabolism in menopausal women. Postgraduate medical journal, 78(926), 727-731. https://doi.org/10.1136/pmj.78.926.727
Li, K., Wang, X. F., Li, D. Y., Chen, Y. C., Zhao, L. J., Liu, X. G., Guo, Y. F., Shen, J., Lin, X., Deng, J., Zhou, R., & Deng, H. W. (2018). The good, the bad, and the ugly of calcium supplementation: a review of calcium intake on human health. Clin Interv Aging, 13, 2443-2452. https://doi.org/10.2147/cia.S157523


Great read . Thank you Kelly